Outline
I. Ethical Frameworks
II. Overview of IVF
III. IVF and Feminist Bioethics
IV. Freezing Embryos
V. Preimplantation Genetic Diagnosis (PGD)
VI. Three Parent Babies
VII. IVF Worldwide
Ethical Frameworks
The Principle of Beneficience
We have an obligation to bring about good in all of our actions. In all cases where we are capable, we must take positive steps to prevent harm.
The Principle of Autonomy
We have an obligation to respect the decisions made by other people concerning their own lives.
The Principle of Nonmaleficence
We have an obligation to not harm others. And, when harm cannot be avoided, we are obligated to minimize the harm we do.
Kantian Ethics
A Kantian framework states that no person can ever be used as a means to an end.
Utilitarianism
A utilitarian framework places the happiness of a society over all else.
Flourishing Society
An idea put forth by philosopher Martha Nussbaum in which a society must meet ten different “capabilities” which she listed as: Life, Bodily Health, Bodily Integrity, Sense, Imagination, and Thought, Emotions, Practical Reason, Affiliation, Other Species (being able to live with other species), Play, and Control over one’s environment (Nussbaum, 1999, p. 41-42).
Overview of IVF
In vitro fertilization (IVF) is a somewhat routine medical procedure ever since the development of the technology in the 1970’s. A female’s eggs are removed with a needle when she is ovulating and the eggs are fertilized in vitro, or in a petri dish. Next, the embryo can either be implanted or saved for future use (Shamoo, et. al., 2009).
IVF and Feminist Bioethics
When I’m with my moms, I say sperm donor, but when I’m with my friends, I say biological father
~S. Baker, child of IVF for lesbian couple
Feminist bioethics can be described as having three main goals which include, “extension of bioethical theory to integrate feminist concerns; development of theory to include analyses not just of gender but also of class, ethnicity and other social categories; and creation of new strategies and methodologies that include socially marginalized experiences and perspectives” (Donchin, et. al., 2015).
Under Feminist bioethics:
- Autonomy is more relational; that is, it is defined more so by relationships and social contexts which influence their opinions (Donchin, et. al., 2015).
- Care ethics uses, “reasoning that prioritizes caring, relationships, and responsibilities” (Donchin, et. al., 2015) which experts argue are more characteristic of women. Conversely, conventional ethics is classified as using, “reasoning that privilege justice and rights” (Donchin, et. al., 2015) which experts say are more characteristic of men.
These characteristics of feminist bioethics can be applied to Baker’s situation. She uses the gap in male attention as a relational way to define her relationship to the sperm donor. She admits she felt a lack of male attention growing up, but does not want to upset her mothers, so she calls him a sperm donor around them. Around her friends, however, she is comfortable to call him a biological father because of her yearning for that fatherly relationship.
Feminist bioethics ties care ethics and conventional ethics together and argues that these bases of ethical principles should not inherently be gendered and that is the flaw in both ethical theories. Using the feminist bioethics combination viewpoint of care ethics and conventional ethics, one can better assess the family dynamic of an IVF child than using one of them alone. The care ethics aspect can assess the relational component of IVF. It forces you to ask the question: is IVF ethical based on the relationships the child will have? Conventional ethics will beg the question: is this fair and just for the parents/ child of IVF?
Freezing Embryos
This short video describes a Missouri couple who were going through a legal battle over their frozen embryos.
Often times more embryos are created than needed and are therefore frozen and stored scientifically known as cryopreservation. This process uses liquid forms of nitrogen to freeze the embryos which can be thawed out and used later. There are more than 600,000 cryopreserved embryos in the nation, according to the U.S. Department of Health and Human Services.
Couples going through IVF often discuss and agree upon what to do with their frozen embryos. In addition, fertility clinics’ paperwork often includes an agreement regarding frozen embryo use. (Persky, 2016). Unfortunately, there are some couples that go through a divorce which may lead to a legal battle over the embryos.
Preimplantation Genetic Diagnosis (PGD)
PGD is the process of testing in vitro fertilized embryos for genetic defects before implanting them into a receptive female. The use of PGD has raised ethical concerns as to whether or not we should be able to select embryos based on their genetic traits.
This video shows the process of IVF and how PGD can be used to identify certain traits of embryos.
How It Works
PGD is a multi-step process. First oocytes (eggs) are retrieved from females who are undergoing controlled ovarian stimulation in which they are producing more oocytes or eggs than normal (Geraedts & De Wert, 2009). These oocytes then undergo IVF or intracytoplasmic sperm injections (ICSI) to form embryos which are then cultured in vitro or out of the body (Geraedts & De Wert, 2009). After 3 to 5 days of culturing, cells are collected from the embryos, as seen in the video by New Hope Fertility Center, and can be screened for genetic defects using a few different techniques. The most common methods of diagnosis include fluorescence in situ hybridization (FISH), a technique where fluorescent probes bind to target regions of DNA for detection as seen in the image below, or a PCR based diagnostic where target sections of DNA can be amplified and analyzed with different tools (Geraedts & De Wert, 2009). Once certain traits are identified, the selected embryos are implanted into a receptive mother where they progress through the normal pregnancy and birthing process.
History and Use of PGD
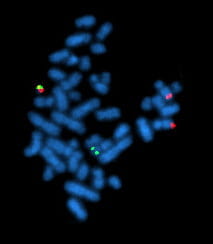
This picture shows the technique of fluorescent in situ hybridization (FISH) being used to mark a chromosomal abnormality associated with chronic myelogenous leukemia. (Wikipedia, 2005)
The process of PGD has been in development ever since first being demonstrated in rabbits in 1968 (Geraedts & De Wert, 2009). PGD was first successfully demonstrated in humans as researchers were able to select the sex of a baby for a couple at risk of transmitting an X-linked disorder (Geraedts & De Wert, 2009). Following this, the same team was able to distinguish embryos with cystic fibrosis mutations and select healthy embryos for implantation (Geraedts & De Wert, 2009). As PGD has developed into a safe and accurate technology, the method has been used to diagnose Mendelian disorders, structural chromosome abnormalities and mitochondrial disorders (Geraedts & De Wert, 2009). In cases of Mendelian disorders, PGD has proven to be 99% effective (Geraedts & De Wert, 2009). As the possibilities of PGD grow, so do the controversial cases and issues surrounding the subject. A high profile case of PGD made news headlines in March of 2008 after a deaf british couple told a BBC reporter that they would like to use IVF and genetic testing technologies to help them have a deaf baby (Lawson, 2008). This sparked outrage and debate over Deaf Culture and whether such use of PGD should be allowed.
PGD And The Possibility For A Better Society
Many argue that PGD violates the ethical principles of justice and human rights as not all embryos are given an equal chance in developing into humans and that discarding embryos is the equivalent of discarding human life. However, if PGD becomes more affordable and widespread in use, individuals and society as a whole would face less suffering and be able to work towards a more utilitarian and flourishing society with greater justice and respect for human rights.
If PGD became more widely available and affordable as well as if society as a whole adopted this technology as common practice, society would see better health and less suffering on a large scale. This idea falls under the concept of a flourishing society. Martha Nussbaum, a philosopher and ethicist has outlined ten key “capabilities” that must be satisfied to reach this idea of a flourishing society. Some of these capabilities include Life, “being able to live to the end of a human life of normal length,” Bodily Health, “being able to have good health,” Bodily Integrity, “being able to move freely from place to place,” and Play, “being able to laugh, to play, to enjoy recreational activities,” (Nussbaum, 1999, p. 41-42). All of these capabilities could become more prevalent in society if PGD were more commonly used to select for offspring less likely to develop certain diseases. Other capabilities defined by Nussbaum such as Emotions, Senses, Imagination,Thought, and control over one’s political and material environment (Nussbaum, 1999, p. 41-42) may be harder to improve with the use of PGD. However one could still argue that better health and less suffering would contribute to people being able to work on improving these areas in their life. So by working towards a society with less suffering and better health, a flourishing society could be achieved or at least become more of a reality than it presently is.
Recent Uses of PGD Disrupt Societal Progress
When PGD was first invented, its sole purpose was to help prevent those parent(s) who are at risk for “severe Mendelian disorders, structural chromosome abnormalities, or mitochondrial disorders” from their offspring carrying the problematic gene (Geraedts et al. 2012). Yet, recently, patients using IVF have been steering towards PGD to engineer embryos simply because they want to decide gender of their child or make sure the child is not intersex. The Medical Encyclopedia defines intersex as “a group of conditions where there is discrepancy between the external genitals and internal genitals” (Kaneshiro, 2015). In many current events, there have been protests and challenges to the government to give rights and acceptance towards those who are born intersex. Many may struggle with this, but many are proud and embrace their differences. The fact that now parent(s) are moving towards eliminating intersex, is taking a step backwards in the progress of the nation. It has been a long battle to get to the place the United States is today, in the movement to eliminate discrimination. So, is this really worth throwing that all away? Aside from preventing a child to be intersex, many patriarchal societies are using and may in the future use this technology to ensure they have a male offspring. This issue is detailed in the Ted Talk below. By ensuring a child is not intersex and a preferential towards males, overall diversity would diminish.
This is a Ted Talk on gender selection, specifically in patriarchal societies (Hendel, 2017).
Affordability of PGD
To ensure a flourishing society, IVF and PGD must be covered by insurance companies and made readily affordable, for sanctioned uses, to those in need of these procedures. Many economic struggles come with procedures such as IVF and PGD. IVF as its own entity is pricey, and some insurance companies refuse to cover the procedure. Furthermore, the additional use of PGD to select the gender of a child adds on three to five thousand dollars (FAQ’s: PGD/IVF, 2016). The limitation put on those who want, or even need such procedures presents an issue that would steer away from a flourishing society. Only the upper class would benefit from this if it was deemed moral, separating the gap from the rich and the poor even further. This major societal gap results in an overall unsatisfied community.In order to prevent such a concern, limitations should be put on the usage of PGD. There should be preliminary screenings and examinations by physicians to ensure that there is a legitimate concern for a severe genetic disease and the cause for use is not simply to identify the gender of the child themselves. Some have argued that pre-implantation genetic diagnosis would be an excellent alternative to prenatal diagnosis. However, prenatal diagnosis tests are far cheaper and covered by the majority of insurance companies. Thus, if this were to be used widely for the sole purpose to prevent a serious disease or disorder, coverage by insurance companies should be considered. Coverage would be a step toward, rather than away, from a flourishing society, where the greater population has the opportunity and care available in an attempt to create healthier lives.
Three Parent Babies
Background
The concept of three parent babies (3PBs) is confusing to many as it has been ill-defined and sensationalized by the media. Simply put, a 3PB has three genetic parents. There are three techniques possible to accomplish this, each varying greatly from the others, but they ultimately all produce children sharing one important characteristic: the child has donor mitochondria that is not from the mother or father (Saey, 2016). Mitochondria, the organelle responsible for producing the molecular energy source for the cell, have their own genome (Kula, 2016; Saey, 2016). Therefore, an otherwise normal embryo containing mitochondria from a donated source will result in a person that technically has three genetic parents. This can have many consequences, as there are over 200 mitochondrial diseases. In the world today there exists 40-60 people with three parents, though a comprehensive understanding of the technology used to create these people is uncommon amongst the general public (Kula, 2016). Of the three techniques available, one is historically the most prevalent, with only two out of 50-60 babies being born with the other techniques. Both babies born by the other techniques are also much more recent and were born just nine months apart, the first being born April 6, 2016 and the second January 5, 2017 (Kula, 2016, Daley, 2017; Saey, 2016).
How It Works
In natural fertilization, the mitochondria are passed from the mother to the child in the egg of the mother (Smith, 2012). In cases where this is not desired, 3PB technology is the solution. The donation of mitochondria must occur outside of the body, meaning that eggs and sperm must be also be removed from the body for fertilization. To fulfill these requirements, in-vitro fertilization (IVF) is done in concert with mitochondrial donation techniques (Masters, 2016). There is one safety risk involved in IVF. Though highly uncommon, it is possible for the mother to develop the potentially life-threatening but treatable condition, ovarian hyperstimulation syndrome, because of the drugs she must be on for IVF to work (“An Outline of Reproductive Technologies,” n.d.). PGD is also routinely done in order to ensure the highest chance of successful embryo implantation. To accomplish mitochondrial donation there exists three different techniques, as previously mentioned. These are: cytoplasmic transfer (CT), pronuclear transfer (PNT), and spindle transfer (ST).
CT is the simplest as well as the most prevalent technique. CT involves extracting 10-15% of donor egg cytoplasm, mitochondria and all, and injecting it into the mother egg along with sperm from the father. PNT and ST are more complex, but can easily be visualized and explained in the following figures (Figure 1 and 2). In these techniques, genetic information is implanted into a whole donor egg via a pronucleus (PNT) or a protein-DNA complex (ST). Both techniques allow for a totally new set of mitochondria to be present and practically no damaged mitochondria from the mother, making them preferable to CT (Saey, 2016).
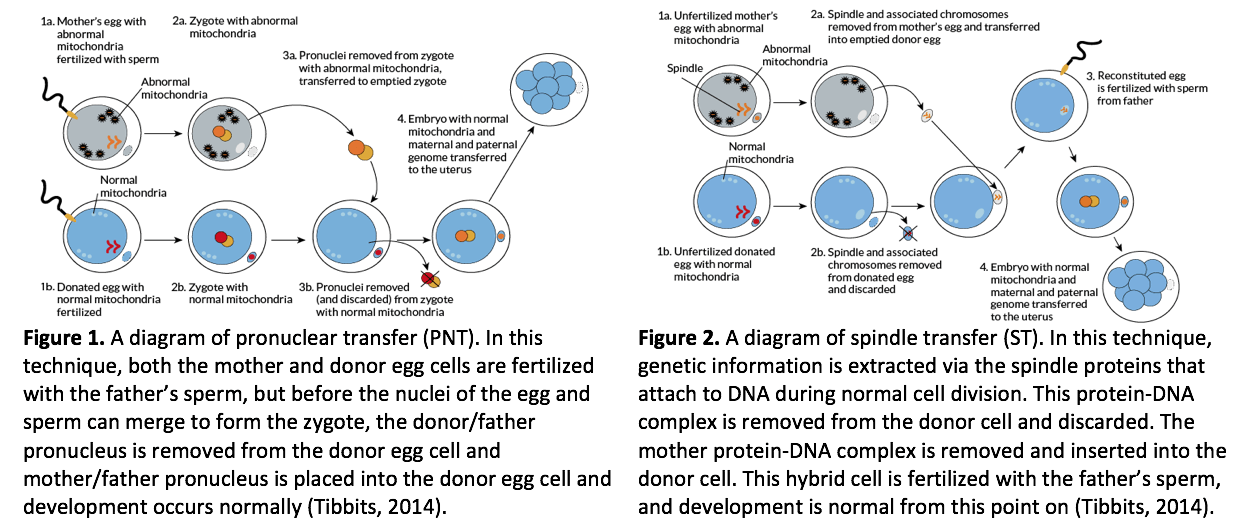
Permission for use of images for educational purposes granted by Science News: https://www.sciencenews.org/permission-republish
Downfalls of These Techniques:
The Problem with CT:
Though CT may seem like a great option given how simple it is, it is also the least effective. In injecting some cytoplasm containing healthy mitochondria into the embryo, the technique can help treat mitochondrial diseases, though overall this is simply adding some healthy mitochondria to a cell with a much greater number of unhealthy mitochondria. This technique isn’t completely ineffective, though the guarantee for curing a mitochondrial disease is not present.
Why Can’t the Father Donate Mitochondria?
At this point you may be thinking, “well why doesn’t the father donate his mitochondria, eliminating the need of a third-party donor? Wouldn’t that accomplish the task of not passing on the mother’s mitochondria and eliminate the confusion of having three genetic parents?” The answer is yes, that would solve those problems, however that is impossible as a male can never be the mitochondrial donor. For the mitochondrial donation into an egg cell to be successful, there must be a plethora of mitochondria donated. Sperm do have mitochondria, though there is such a small amount it would not be effective in aiding in the development of a healthy, mitochondria-filled embryo (Smith, 2012). In addition, this describes the same problem as found in CT: this is simply adding some healthy mitochondria to a cell with a much greater number of unhealthy mitochondria.
Ethical Issues Outlined:
Curing Disease:
There are over 200 mitochondrial diseases. Because mitochondria contain their own genome and are physically transferred into the baby from the mother, eliminating the presence of the damaged mitochondria and replacing them with donor mitochondria is the only cure for all 200 of these diseases. There is no other cure for any mitochondrial disease (Fox, 2016). Without 3PB technology, the child of a mother who has damaged mitochondria will have either a long life of debilitating illness or a death sentence. But we have the technology to stop this from happening, and in doing so eliminate the suffering of a future child before it begins.
Now, are we obligated to use this technology? The principle of beneficence applies here, in stating we must take positive steps to prevent harm when possible. By only following that principle, it seems we are, without a doubt, obligated to use 3PB technology. This comes into direct conflict, however, with the principle of autonomy. According to this principle, it may seem that the mother could not be forced undergo these procedures and endure the risks involved, though it may save the child. However, this view of autonomy also discounts the future child’s autonomy—if there was a choice for the child to forego his or her illness, never having to be afflicted for even one day, is there any doubt that they would chose this? The situation now appears as though there is no situation in which autonomy is not violated, and there is no scenario where no possible harm occurs, either to the mother or child. Therefore, we must turn to the principle of nonmaleficence, stating that when harm cannot be avoided, we are obligated to minimize the harm that we do. With this in mind, it is quite clear that the potential risks to the mother of creating a 3PB are severely outweighed by the alternative of having of a baby with damaged mitochondria. Therefore, it is most ethical that in all cases where a mitochondrial disease may be passed on to a child, 3PB technology should be used to eliminate that possibility.
The Use of Multiple Embryos:
Another issue that arises in creating 3PBs is in the technology’s inherent need for multiple eggs. For convenience sake, I will not be discussing CT as it is an overall ineffective technique. At the very least, one egg is used for nothing other than to donate either a pronucleus (PNT), or a protein-DNA complex (ST) (Saey, 2016). In using eggs this way, one may jump into an argument defined around Kantian ethics, stating that no person can be used a means to an end. For a productive argument around this framework, a definition must first be made of when one considers life to begin. The most constricting stance is that life begins at fertilization, thus this will be what we frame our argument around. With this view of life, only PNT is a problem in this Kantian argument. PNT involves fertilizing both the mother egg and the donor egg, as previously described. This means that only one of those two fertilized eggs finally develops into a full zygote and the other fertilized egg is discarded, using a person for nothing more than a means to an end. In ST, however, no fertilization occurs before the transfer of the protein-DNA complex occurs. An egg is certainly still used up and discarded for another egg to successfully survive, though this is merely a single cell being used and not what we have defined as a person. Therefore, the use of ST is not in conflict with the Kantian argument. For those individuals who define life as beginning at fertilization, PNT is unethical and should not be used, though the ST method still exists for these individuals to create a 3PB. Even within this constrictive framework, there is still an option for 3PB technology to be ethically sound.
In defense of PNT, one could use a utilitarian framework to combat this Kantian argument, stating that the overall maximum happiness is achieved in sacrificing this one potential embryo to create a healthy, embryo that would develop into a mitochondrial-disease-free human. A requirement for this argument, however, is that PNT is the only option available, because if ST is available then the maximum happiness can be achieved without requiring the sacrifice of an embryo.
Future Ethical Issues to be Considered:
- Who is legal mom and dad?
- Does the mitochondrial donor have legal grounds for custody of the child?
- Feminist bioethics would apply here using care ethics to argue for what a true parent may be, more than just a supplier of biological material
- Special case of PNT baby. This was done because of infertility instead of mitochondrial disease (Daley, 2017).
- Does infertility warrant the use of 3PB technology?
- If child born is female, if she has children then she will pass on the donor mitochondria.
- All of her children will have three genetic parents, how does that original mitochondrial donor relate to the new children?
- Feminist bioethics applies here in extending the discussion of a mitochondrial donor’s care responsibilities to all of that original recipient’s progeny
IVF Worldwide
Fertility tourism is the Idea of going abroad to obtain IVF, or related procedures. At a success rate of roughly 30%, some reasons women seek IVF are age, infertility, surrogacy, and acquiring a specific genetic outcome are of the most common. Many factors such as price, biobank regulations, laws, and religious prevention are all reasons people might seek to go abroad. (Top Destinations) In countries under Islamic law IVF is permitted only for married couples. Seeing that in Costa Rica Catholicism is the state religion, it was the last remaining country in the world with a country wide ban on IVF. (Mora-Bermúdez 2016) Laws and regulation also play a role in fueling fertility tourism. In Germany, embryos cannot be frozen, discouraging Germans to seek native IVF. While gay couples seek IVF across the world, France is not a place that allows lesbians access to a biobank, so they often travel next door to Norway, where they do allow it. (Laurance 2011) Germany does not accept Surrogacy, so when a couple took their embryos to India, the child was denied citizenship when the parents tried to return home with their newborn twins. The Indian surrogate was listed as their biological mother on the birth certificates, and the case was taken to the Supreme Court of New Delhi, in order to grant the twins travel papers back to Germany. Even when parents think they do everything right, these things happen, and it can affect the child for the rest of their lives. (Whelan 2014)
A flourishing society seeks to ask what can be done differently, or how can the society be improved, as opposed to a ‘what are we doing wrong’ mindset. (Nussbaum) These regulations associated with IVF are in support of setting up an ideal flourishing society in the eyes of country in question. As Kurzweil quotes, “An analysis of the history of technology shows that technological change is exponential, contrary to the common-sense ‘intuitive linear’ view”, meaning that technology is rapidly improving, and scientists are achieving goals we thought never imaginable, including IVF. This technology is rapidly developing, opening a wide range of possible treatments (Kurzweil). The regulations are there to protect women from risks such as ectopic pregnancy, miscarriages, cancer, and birth defects, so they don’t end up like ‘octomom’ the woman who had 8 embryos implanted, and they all took (Mayo clinic).
Work Cited
“Alana Saarinen at the Piano.” (2014). [Digital Image]. 2017. http://www.bbc.com/news/magazine-28986843.
“An Outline of Reproductive Technologies.” N.p.: n.p., n.d. 104-06. Web.
Fox, M. (2016, February 3). Three-Parent Babies Are OK, Experts Say. NBC, p. Health. Retrieved from http://www.nbcnews.com/health/health-news/three-parent-babies-are-ok-experts-say-n510626
“Clinic director Valery Zukin holding the baby girl.” (2017, January). [Digital Image]. 2017. https://www.newscientist.com/article/2118334-first-baby-born-using-3-parent-technique-to-treat-infertility/.
Donchin, Anne and Scully, Jackie, “Feminist Bioethics”, The Stanford Encyclopedia of Philosophy (Winter 2015 Edition), Edward N. Zalta (ed.), URL = <https://plato.stanford.edu/archives/win2015/entries/feminist-bioethics/>.
Education and Research, 16 June 2016. Web. 03 Apr. 2017. <http://www.mayoclinic.org/tests-procedures/in-vitro-fertilization/details/risks/cmc-20207080>.
FAQs: PGD/IVF Gender Selection Cost & Other Q/A | Gender Baby. (2016). Retrieved April 11, 2017, from http://www.gender-baby.com/faqs/
Geraedts, J. P. M., & De Wert, G. M. W. R. (2009). Preimplantation genetic diagnosis. Clinical Genetics, 76(4), 315–25. https://doi.org/10.1111/j.1399-0004.2009.01273.x
Goldsammler, M., & Jotkowitz, A. (2012). The Ethics of PGD: What About the Physician?: Books, Articles, & More… The American Journal of Bioethics, 12(4), 28–29. Retrieved from http://eds.b.ebscohost.com/eds/pdfviewer/pdfviewer?sid=566c9cdb-a4f2-4387-a74d-5f8adb45017f%40sessionmgr103&vid=0&hid=108
Hendel, T. (2017, April 10). Challenging Gender Selection. Lecture presented at TEDxMacquarieUniversity in Australia, Sydney. Retrieved April 10, 2017, from https://www.youtube.com/watch?v=eZg-GgToBEE
“John Zhang Holds a Baby Boy.” (2016, October). [Digital Image]. 2017. https://www.sciencenews.org/article/three-parent-babies-explained.
Kaneshiro, N. (2015, July). Intersex. Retrieved April 12, 2017, from https://medlineplus.gov/ency/article/001669.htm
Kolata, G. (2014, February 3). Ethics Questions Arise as Genetic Testing of Embryos Increases. Retrieved April 5, 2017, from https://www.nytimes.com/2014/02/04/health/ethics-questions-arise-as-genetic-testing-of-embryos-increases.html
Kula, S. (2016, February). Three-Parent Children Are Already Here. Slate. Retrieved from http://www.slate.com/articles/technology/future_tense/2016/02/three_parent_babies_have_been_here_since_the_late_90s.html
Kurzweil, Ray. “KurzweilAI | Accelerating Intelligence.” KurzweilAI The Law of Accelerating Returns Comments. N.p., n.d. Web. 12 Apr. 2017. <http://www.kurzweilai.net/the-law-of-accelerating-returns>. (Taken from Human Enhancement reading)
Laurance, Health Editor Jeremy. “Study Highlights Dangers of IVF Treatment Overseas.” The Independent. Independent Digital News and Media, 23 Oct. 2011. Web. 30 Mar. 2017. <http://www.independent.co.uk/life-style/health-and-families/health-news/study-highlights-dangers-of-ivf-treatment-overseas-2078447.html>.
Mayo Clinic Staff Print. “In Vitro Fertilization.” Mayo Clinic. Mayo Foundation for Medical Donchin, Anne and Scully, Jackie, “Feminist Bioethics”, The Stanford Encyclopedia of Philosophy (Winter 2015 Edition), Edward N. Zalta (ed.), URL = <https://plato.stanford.edu/archives/win2015/entries/feminist-bioethics/>.
Masters, J. (2016, December 15). “Three-Parent” Babies Approved in the UK. CNN. Retrieved from http://www.cnn.com/2016/12/15/health/babies-three-people-embryos/
Mora-Bermúdez, Felipe. “Costa Rica: World’s Last in Vitro Fertilization Ban Falls.” Nature News.
Nature Publishing Group, 17 Aug. 2016. Web. 04 Apr. 2017. <http://www.nature.com/nature/journal/v536/n7616/full/536274c.html?WT.ec_id=NATURE-20160818&spMailingID=52085095&spUserID=MjA1NzUwNjc4NgS2&spJobID=983154956&spReportId=OTgzMTU0OTU2S0>.
Nussbaum, M. C. (1999). Sex & social justice. Oxford: Oxford University Press.
Persky, A. S. (2016). Contentious battles between couples over frozen embryos raise legal and ethical dilemmas. ABA Journal, 8.
Saey, T. H. (2016). “Three-Parent Babies” Explained: IVF Technique that Led to Recent Birth of Boy One of Several. Retrieved from https://www.sciencenews.org/article/three-parent-babies-explained
Smith, J. (2012). Do Fathers Pass on mtDNA? Retrieved April 12, 2017, from http://genetics.thetech.org/ask-a-geneticist/mtdna-comes-only-mom
Tibbits, T. (2014, June). Human Fertilization and Embryology Authority. Pronuclear Transfer [Digital image]
Tibbits, T. (2014, June). Human Fertilization and Embryology Authority. Spindle Transfer [Digital image].
“Top Destinations for Fertility Treatment.” Fertility Treatment Abroad. N.p., n.d. Web. 12 Apr. 2017. <http://fertility.treatmentabroad.com/countries>.
Whelan, Corey. “What Is the Risk and Ethics of Reproductive Tourism.” Global IVF Medical Fertility Tourism. N.p., 27 May 2014. Web. 05 Apr. 2017. <http://globalivf.com/2012/10/21/reproductive-tourism-risks-and-ethics/>.
About the Authors
Brooke, Colin, Rachel, Sabrina, Shaw, and Tryphena are studying the use of In Vitro Fertilizaiton, and designer babies in todays society. They have been working to put together this Word Press page in order to use various ethical frameworks to analyze the use of this new technology. Together they make up the Bioethics Group in their ISAT 456 course, Ethical, Legal, and Social Implications of Biotechnology, in one of the largest schools in Virginia, James Madison University.
Disclaimer: This was a collaborative class project that represents multiple viewpoints. Some views may not be shared by all contributors to this page
